Assessing potential missed opportunities for recommended clinical care among users of GetCheckedOnline, British Columbia’s online testing service for sexually-transmitted and blood-borne infections.
Research theme(s)
Internet Based Testing
Mark Gilbert,1,2 Aidan Ablona,1,2 Hsiu-Ju Chang,1,2 Ihoghosa Iyamu,1,2 Devon Haag,1 Heather Pedersen,1 Gina Ogilvie,2,3 Troy Grennan.1,2
1. BC Centre for Disease Control, 2. University of British Columbia, 3. BC Women’s Hospital.
STI & HIV World Congress 2023, July 24-27, 2023, Chicago, IL, USA.
Background:
- Online testing services for sexually-transmitted and blood-borne infections (STBBI) are usually intended for people who are asymptomatic, typically recommending that people with symptoms or partners with an STI seek clinical care as empirical treatment or other tests not included in the online testing service may be needed.
- The same is true for GetCheckedOnline (GCO), BC’s digital STBBI testing service, where users indicating symptoms or a partner with an STI are routed to a webpage that recommends the user see a healthcare provider but still allows the user to proceed with testing if they choose. In 2022, 17% and 7% of GCO users completing testing indicated they tested while symptomatic or with a partner with an STI, respectively.
- Further modifications in 2021 provided additional messaging to users who chose to proceed with testing and had negative results, which repeats the recommendation to seek clinical care. However, the extent to which users of GCO speak to healthcare providers in this scenario is not known.
- We wanted to better understand how common these potential missed opportunities for recommended clinical care occurred, and whether this was related to barriers accessing provider-based testing we know to be common among GCO users.
Methods:
- This secondary analysis is part of an online survey that invited GCO users who had created an account or tested between April 7 and October 7, 2022, and consented to research. Participants were provided with a $20 CDN honorarium. The survey was approved by the UBC Behavioural Research Ethics Board.
- Survey domains included ever testing through GCO when had symptoms or a partner with an STI, test results, and speaking with a health care provider at the time (outcomes of interest), as well as questions related to barriers accessing healthcare providers for testing.
- We described the frequency of outcomes among all participants who had completed at least one test through GCO.
- We further restricted our analysis to participants reporting ever testing while symptomatic or having a partner with an STI and having a negative result. We conducted bivariate analyses between speaking with a provider at the time and variables related to barriers accessing healthcare providers for testing (using chi-squared tests, significance set at p<0.05).
Results:
- Of 4926 GCO users invited, 1524 (31%) responded with 1224 participants having testing at least once through GCO and included in this analysis (25% once, 20% two times, 26% 3-4 times, 29% more than five times).
Figure: Categorization of survey participants by outcomes of interest
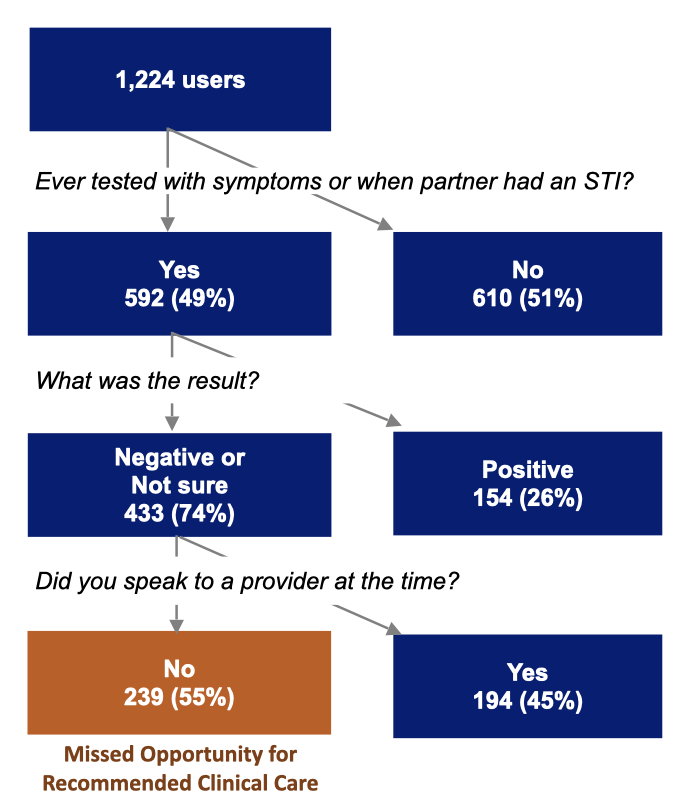
Table: Results of bivariate analysis among 433 participants testing through GCO while symptomatic/partner with an STI and having a negative test result
|
Spoke to HCP at the time? |
Yes (N=194) |
No / Not sure (N=239) |
p-value |
|
Comfort discussing sexual history with HCP (Very uncomfortable/uncomfortable vs. not) |
16% |
27% |
0.013 |
|
Anxious in waiting rooms when I go to a clinic to get tested (Strongly agree/agree vs. not) |
38% |
42% |
0.506 |
|
Worry about being judged by HCP when providing information about sexual history (Very worried/somewhat worried vs. not) |
33% |
41% |
0.117 |
|
Usual location when need care for a minor health problem (A doctor or nurse practitioner’s office vs. not) |
53% |
46% |
0.178 |
|
Have a family doctor or nurse practitioner (Yes vs. no/not sure) |
66% |
57% |
0.069 |
|
Have usual place where comfortable getting tested by HCP (Strongly agree/agree vs. not) |
53% |
38% |
0.003 |
|
Easy to see a HCP for testing when need to (Strongly agree/agree vs. not) |
26% |
26% |
1.000 |
|
More convenient to test through HCP than GCO (Strongly agree/agree vs. not) |
21% |
20% |
0.983 |
|
Have more privacy if test through GCO compared to HCP (Strongly agree/agree vs. not) |
69% |
79% |
0.032 |
Notes: HCP = healthcare provider. Missing responses for each variable excluded from percentages.
Conclusion:
- In this exploratory study, we found that 20% (239/1224) of participants testing at least once through GCO had ever tested while symptomatic/partner with an STI, had a negative test result and did not speak with a provider at the time.
- Not speaking with a provider may in part be related to barriers accessing provider-based testing. We found discomfort discussing sexual history, not having a usual place where comfortable getting tested, or perceiving testing through a provider as less private significantly associated with these potential missed opportunities for recommended clinical care.
- These findings reinforce the ongoing challenges in accessing healthcare providers for testing among users of digital testing services (which is often their motivation for use of these services), and improving access to provider-based testing may help to reduce this clinical gap.
- Further research to better understanding the contexts of these potential missed opportunities for recommended clinical care may help identify whether further service adaptations may also be needed.
